After months of delay, Northern Health’s President and Chief Executive Officer, Ciro Panessa was at last able to attend the Peace River Regional District’s board of directors meeting on March 6 to provide an update on what the health authority is doing to improve the delivery of health services in northeastern British Columbia.
Throughout the presentation, while they welcomed news of improvements, directors expressed their concerns about some aspects of Northern Health’s strategic plan to improve the delivery of healthcare services in the Northeast.
Pouce Coupe director and mayor Danielle Veach’s concern was that the virtual hybrid model would put additional pressure on sectors of the system such as X-ray Technicians and the labs.
“It’s too early to say,” Panessa responded, noting that there would be more pressure on nursing teams and that’s another reason they’re trying to increase the number of nurses in Northern Health.
Area E director Dan Rose said that the relationship between patients and doctors is important for a lot of people, and that digitizing medical records will cause problems for seniors, “who aren’t going to have their medical records in their phones.”
“We need boots on the ground.”
Fort St. John director Tony Zabinsky pointed out that there are doctors who just want to be doctors, general practitioners who don’t want to work in hospitals. He said he understands the move to the digital options, but as Director Rose said, “we have to have boots on the ground.”
The model needs to be changed to allow doctors to be doctors, Zabinsky said.
“For the seniors, or someone who’s still in his community, could go knock on the door, make his appointment and see his doctor – if you could change that, the doctor could just be a doctor and not do everything else.”
Panessa agreed that there needs to be a balance between the types of the medical services in the community, while maintaining minimum service levels in the hospital and the community.
“What’s the individual practice look like for everyone to be workable for them personally but also contribute to a whole service model.”
Directors still had concerns and at the end of the board meeting, Tumbler Ridge director and mayor Darryl Krakowka brought forward a notice of motion requesting “staff investigate the hiring of doctors as PRRD employees as per Colwood, BC and bring back a report on the pilot program.”
In December 2024, the City of Colwood launched a pilot project to directly hire family physicians to ensure that all the city’s residents could access primary health care. The first doctor arrived in January and the goal of the project is to eventually hire seven more doctors to serve the city’s 10,000 residents.
Stabilizing ERs is Northern Health’s top priority
Panessa’s presentation highlighted the positive changes that are occurring in Northern Health and the Northeast in particular.
Health and human resourcing, Panessa said “continues to be the biggest risk in terms of us being able to achieve our mandate as a health service delivery organization and meeting the expectations of all those that live in northeastern British Columbia.”
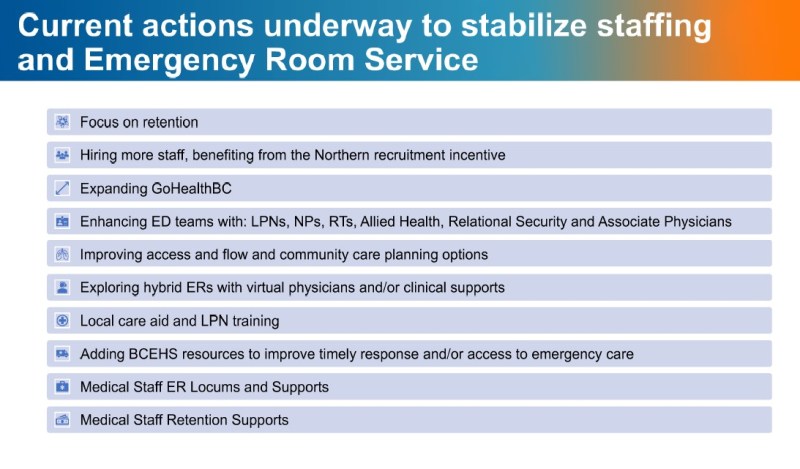
Northern Health’s current areas of focus include stabilizing ER’s, maternity and psychiatry services; improving surgery; bolstering primary and community care, including seniors care; benefitting from digital enhancement; the ongoing drug crisis and worsening life expectancy; and completing major capital redevelopments.

“ERs understandably continue to be one of our top issues that we’re looking to stabilize,” he added.
The biggest tool in Northern Health’s toolbox is GoHealthBC, Panessa said.
GoHealthBC is “our own essentially in-house travel nurse program. They’re not external contracted agencies. They are Northern Health employees, but they travel around to communities across the North.”
The majority of GoHealthBC nurses come from outside Northern BC, so Panessa says that means they’re bringing new nurses into Northern BC.

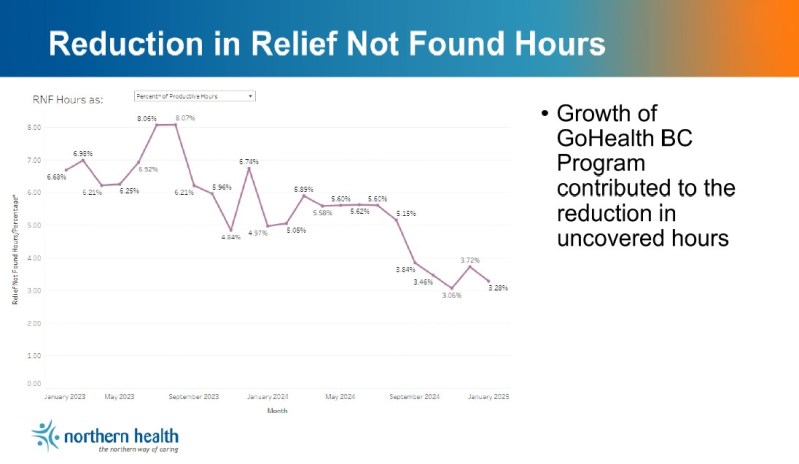
It “creates an opportunity to work our magic in terms of getting people to set up shop, or live, or deciding to move, start a family and a life in Northern BC,” he said.
Of the northeastern communities, Fort St. John is benefitting the most from GoHealthBC nurses, receiving twice as many hours of service from GoHealthBC nurses compared to Dawson Creek. The program has contributed to a reduction in the number of uncovered hours in ERs, and less ER closures in the two communities.
Although there is still a high vacancy rate in nursing in Northern Health – 27 percent overall and 42 percent in ER’s – the Northeast is something of an outlier with vacancy rates of 20 percent overall and 29 percent in the ER’s.
The number of emergency room closures is dropping, according to Northern Health and there is a consistent downward trend in the number of nurse-related “service interruptions”. Most closures are now due to physician shortages.
While some communities are doing quite well with recruitment and retention of doctors, others don’t have close to the recommended number of physicians.
Northern Health is looking at bringing other types of providers into the mix to keep services going, such as virtual hybrid options and associate physicians.
An associate physician is one who was trained outside of Canada, and not yet licenced in British Columbia. These doctors work along side other doctors, under supervision in a role very similar to a resident physician, until such time as they can get licenced to practice in BC.
The virtual hybrid model relies on nursing staff to interact with patients, so Panessa says the “nursing piece” would have to be increased along with switching to a virtual model.
Local training for nurses is key to filling the need for nursing staff, and Panessa says Northern Health is grateful to Northern Lights College, which has been an outstanding partner through the Baccalaureate Nursing Program.
The health authority is also looking at a rapid practical nursing initiative and is working with NLC to get the LPN training program down from 18 to 24-months to just 13 months.
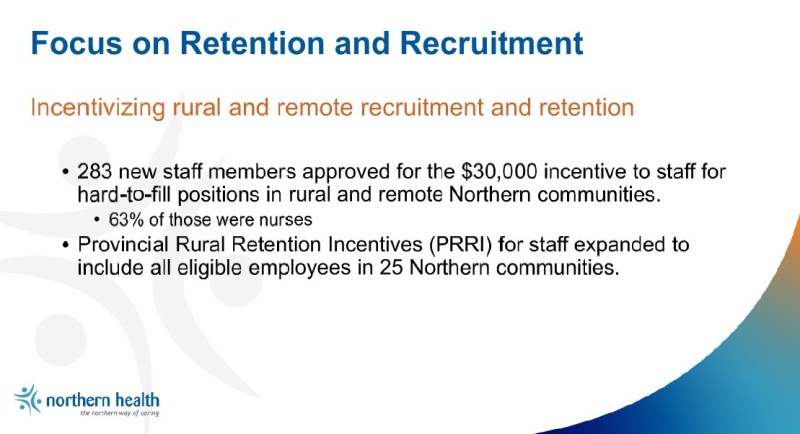
Locum coverage is another way Northern Health is addressing the shortage of doctors. By having a locum come in – a doctor from other parts of the province who comes in to provide relief for local physicians – permanent doctors can have a break, such as for scheduled vacations. The problem with relying on locums comes where some communities have over 25 percent locum coverage, sometimes up to 50 percent, creating instability in schedules.

Long waitlists and wait-times for surgeries are problems that have plagued the province in recent years. However, the number of surgeries being performed in Northern Health are getting back to pre-pandemic levels, due to the increasing ability to get enough people to form surgical teams, and deal with the backlog, according to Panessa.


Have an insight or additional info regarding this article? Feel free to drop a comment!